An increase in the frequency of antibiotic resistance in bacteria since the 1950s has been observed for all major classes of antibiotics used to treat a wide variety of respiratory illnesses, skin disorders, and sexually transmitted diseases. Is this resistance the result of bacteria evolving new genes in response to the presence of antibiotics, or are antibiotic-resistant bacteria selected for in the environment by possessing antibiotic resistance genes beforehand? To answer these questions a discussion of several factors involved in antibiotic resistance will show that resistance is a designed feature of pre-existing genes enabling bacteria to compete with the antibiotic producers in their environment.
A brief look at an example of penicillin resistance reveals the increase in the frequency of antibiotic-resistant organisms since the time when antibiotic use became common. Penicillin is an antibiotic produced by the common bread mold Penicillium that was discovered accidentally in 1929 by the British microbiologist, Alexander Fleming. By the 1940s, penicillin was available for medical use and was successfully used to treat infections in soldiers during World War II. Since then, penicillin has been commonly used to treat a wide range of infections. In 1967 the first penicillin-resistant Streptococcus pneumoniae was observed in Australia, and seven years later in the U.S. another case of penicillin-resistant S. pneumoniae was observed in a patient with pneumococcal meningitis.[1] In 1980 it was estimated that 3-5% of S. pneumoniae were penicillin-resistant and by 1998, 34% of the S. pneumoniae sampled were resistant to penicillin.1 Antibiotic resistance by other organisms reflects the same trend observed between S. pneumoniae and penicillin. Tetracycline resistance by normal human intestinal flora has exploded from 2% in the 1950s to 80% in the 1990s.[2] Kanamycin, an antibiotic used in the 1950s, has become clinically useless as a result of the prevalence of kanamycin-resistant bacteria. The increase in resistance among these organisms clearly indicates a change in the frequency of antibiotic resistance genes.
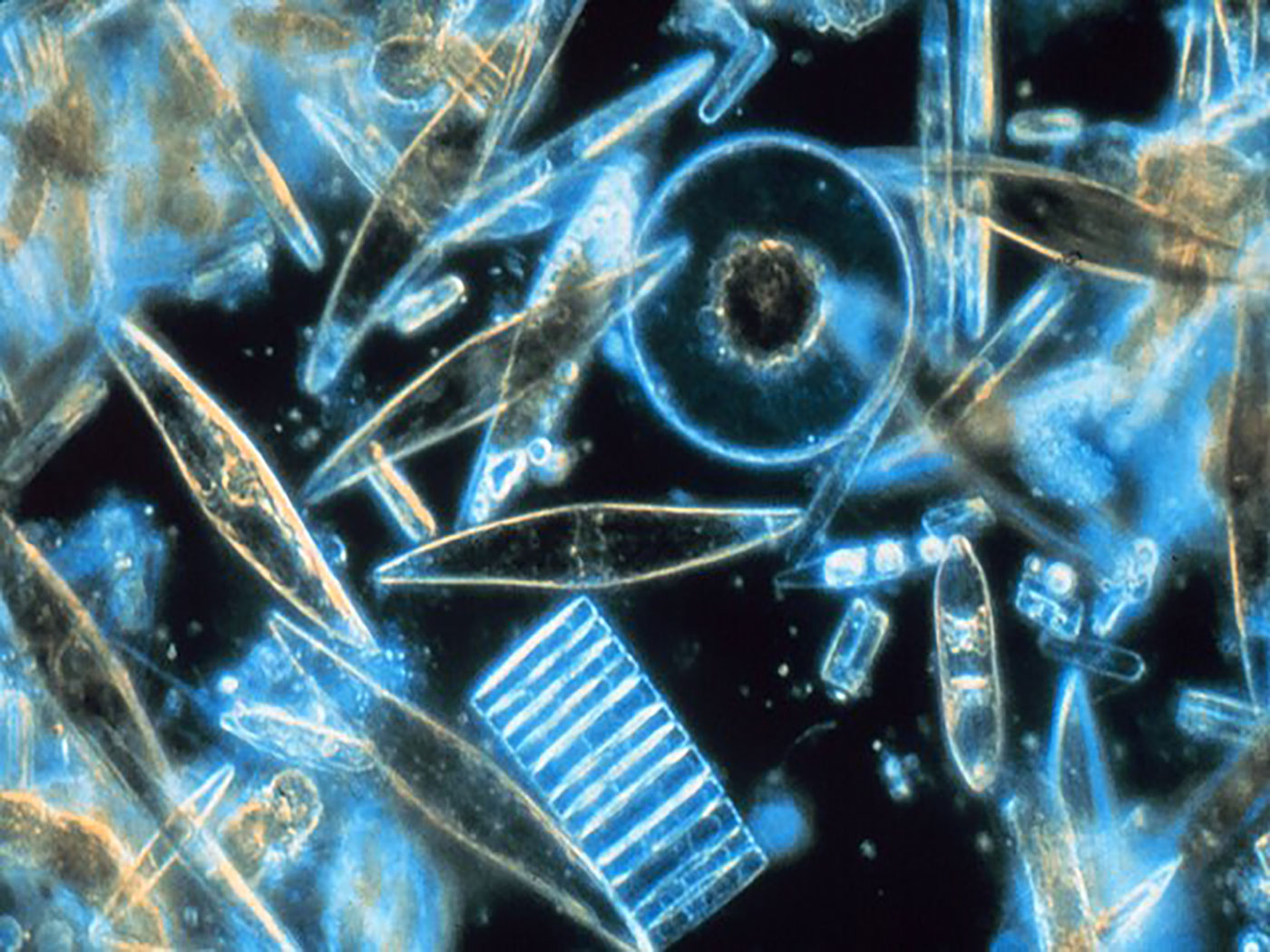
Since World War II many more antibiotics isolated from fungi (molds) and bacteria have been used to treat a wide range of human and animal infections. One group of bacteria, the Streptomyces, produces most of the medically important antibiotics.[3] Streptomyces release antibiotics into the soil in a sort of "biochemical warfare" scenario to eliminate competing organisms from their environment. These antibiotics are small molecules that attack different parts of an organism's cellular machinery. Streptomyces-produced quinolone and coumarin antibiotics, such as novobiocin, interfere with a protein called gyrase that assists in the normal separation of double-stranded DNA during replication of DNA or transcription of messenger RNA.[4] Failure of DNA to properly separate during these processes results in a bacterium not being able to divide normally or produce functional proteins. Ribosomes, the structures where protein synthesis is catalyzed, are the targets of many other Streptomyces antibiotics such as spectinomycin, tetracycline, and streptomycin. Spectinomycin and tetracycline prevent proteins from being assembled by the cell and streptomycin induces the assembly of the wrong amino acids into the translated protein.[5,6] Without proteins, which are necessary for normal cell function, the cell dies. The slight differences between human ribosomes which are not bound by these antibiotics and bacterial ribosomes make this type of antibiotic ideal for treating many illnesses. Other antibiotics, such as penicillin, block the assembly of the bacterial cell wall causing it to weaken and burst.[7] Penicillin is an effective antibiotic for human diseases because it interferes with a biological component in bacteria (cell wall) not found in human cells. The production of antibiotics by these organisms provides them with a competitive advantage over non-resistant bacteria in their environment. Just as large organisms such as plants and animals must compete for living space, food, and water, these microbes use antibiotics to eliminate competition with other microbes for these same resources.
However, not all bacteria are defenseless against the antibiotic producers. Many possess genes that encode proteins to neutralize the affects of antibiotics and prevent attacks on their cell machinery. Efflux pumps, located in the cell membrane, are one method of protection that many bacteria use against the influx of antibiotics.[6] The offensive antibiotic is pumped out of a cell that possesses these pumps before the antibiotic can cause harm to the cellular machinery. Although many efflux pumps may be specific for the substrate they pump out of the cell, they are not uncommon. Ribosomal protection proteins (RPP) are another source of resistance bacteria use to protect themselves from antibiotics. These proteins protect ribosomes by binding them and changing their shape or conformation. The change in the ribosome shape prevents an antibiotic from binding and interfering with protein synthesis.6 The RPP-bound ribosomes are able to function normally during protein synthesis, an important feature of this method of antibiotic resistance. Some bacteria produce enzymes that neutralize antibiotics by adding acetyl (COCH3) or phosphate (PO32-) groups to a specific site on the antibiotic.[8] This modification reduces the ability of the antibiotic to bind to ribosomes, rendering it harmless to the cell.[9] Interestingly, all three types of antibiotic-resistant genes that produce efflux pumps, ribosomal protection proteins, and modifying enzymes are found in Streptomyces species, the producers of many antibiotics. It appears this is the method Streptomyces uses to protect itself from its own antibiotics.
Is it possible to transfer these resistance genes to other bacteria? A unique bacterial characteristic that has not been demonstrated in plant and animal cells is the ability to transfer genes from one bacterium to another, a process called lateral gene transfer. Genes located on a circular strand of DNA called an R-plasmid may contain several antibiotic-resistant genes. Through a process called conjugation an antibiotic-resistant bacterium can transfer the antibiotic resistance genes from an R-plasmid to a non-resistant bacterium.[10] Ironically, several antibiotic resistance genes found in other pathogenic bacteria are very similar in DNA sequence to the genes found in Streptomyces species.[11] The efflux pumps that Streptomyces use to pump out antibiotics to eliminate their competitors are likely the same pumps that other species of bacteria are now using to pump out the offensive antibiotic delivered from Streptomyces! The antibiotic-resistant bacteria likely have acquired the genes for these efflux pumps through lateral gene transfer. The presence of ribosomal protection proteins and antibiotic modifying enzymes in resistant bacteria has also likely originated from Streptomyces or some other antibiotic-producing microbe.6 Bacteria don't appear to be evolving new genes; they are acquiring previously existing antibiotic resistance genes through lateral gene transfer. This allows a species of bacteria to possess enough genetic variability to adapt to a changing environment and to compete with its neighbors. (This method of defense is very similar to the genetic variability of mammalian antibody-producing B lymphocytes—a topic for another Impact article.) The bacterium that acquires the antibiotic resistance genes still has the physical and metabolic qualities that distinguish it from other bacteria kinds and associates it with its own kind of bacteria. The observed increase in the frequency of antibiotic-resistant bacteria has resulted from the increased use of antibiotics in medicine and agriculture, resulting in the reduction of organisms that do not possess antibiotic resistance genes.
Antibiotic resistance in bacteria can also be achieved when mutations in a ribosome or protein change the site where an antibiotic binds. For example, four of the antibiotics mentioned earlier, tetracycline, streptomycin, kanamycin, and spectinomycin, bind to a specific region of a ribosome and interfere with protein synthesis. Mutations may prevent an antibiotic from binding to the ribosome (kanamycin)[12] or allow the ribosome to function even while the antibiotic is bound (streptomycin and spectinomycin).[5] Although it appears these mutations are beneficial and provide an advantage to the bacterium possessing them, they all come with a cost. Ribosomal mutations, while providing antibiotic resistance for the organism, slow the process of protein synthesis, slow growth rates, and reduce the ability of the affected bacterium to compete in an environment devoid of a specific antibiotic.[13,14] Furthermore, a mutation that confers resistance to one antibiotic may make the bacterium more susceptible to other antibiotics.[15] These deleterious effects are what would be expected from a creationist model for mutations. The mutation may confer a benefit in a particular environment, but the overall fitness of the population of one kind of bacterium is decreased as a result of a reduced function of one of the components in its biological pathway. The accumulation of mutations doesn't lead to a new kind of bacterium—it leads to extinction.
References
- Doern, G.V. et al., 2001. Antimicrobial resistance among clinical isolates of Streptococcus pneumoniae in the United States during 1999_2000, including a comparison of resistance rates since 1994-1995. Antimicrobial Agents and Chemotherapy 45(6)1721-1729.
- Shoemaker, N.B. et al., 2001. Evidence for extensive resistance gene transfer among Bacteriodes spp. and among Bacteriodes of other genera in the human colon. Applied and Environmental Microbiology 67:561-568.
- Tanaka, Y., and S. Omura, 1990. Metabolism and products of actinomycetes: an introduction. Actinomycetologica 4:13-14.
- Contreras, A., and A. Maxwell, 1992. gyrB mutations which confer coumarin resistance also affect DNA supercoiling and ATP hydrolysis by Escherichia coli DNA gyrase. Molecular Microbiology 6(12):1617-1624.
- Carter, A.P. et al., 2000. Functional insights from the structure of the 30S ribosomal subunit and its interactions with antibiotics. Nature 407:340-348.
- Chopra, I., and M. Roberts, 2001. Tetracycline antibiotics: mode of action, applications, molecular biology, and epidemiology of bacterial resistance. Microbiology and Molecular Biology Reviews 65(2):232-260.
- Garrett, R.H., and C.M. Grisham, 1999. Biochemistry 2nd ed., Saunders College Publ., New York.
- Wright, G.D., 1999. Aminoglycoside-modifying enzymes. Current Opinion in Microbiology 2:499-503.
- Llano-Sotelo, B. et al., 2002. Aminoglycosides modified by resistance enzymes display diminished binding to the bacterial ribosomal aminoacyl-tRNA site. Chemistry and Biology 9:455-463.
- Campbell, N.A., and J.B. Reece, 2002. Biology 6th ed. Benjamin Cummings, Publ. San Francisco.
- Benveniste, R., and J. Davies, 1973. Aminoglycoside antibiotic-inactivation enzymes in actinomycetes similar to those present in clinical isolates of antibiotic-resistant bacteria. Proceedings of the National Academy of Sciences USA 172:3628-3632.
- Recht, M.I. et al., 1999. Basis for prokaryotic specificity of action of amino-glycoside antibiotics. EMBO Journal 18(11):3133-3138.
- Zengel, J.M. et al., 1977. Role of ribosomal protein S12 in peptide chain elongation: analysis of pleiotropic, streptomycin-resistant mutants of Escherichia coli. Journal of Bacteriology 129:1320-1329.
- Gregory, S.T. et al., 2001. Streptomycin-resistant and streptomycin-dependent mutants of the extreme thermophile Thermus thermophilus. Journal of Molecular Biology 309:333-338.
- Recht, M.I., and J.D. Puglisi, 2001. Aminoglycoside resistance with homogeneous and heterogeneous populations of antibiotic-resistant ribosomes. Antimicrobial Agents and Chemotherapy 45(9):2414-2419.
* Dr. Daniel Criswell has a Ph.D. in Molecular Biology.